Va Secondary Claim Denied
If you're searching for video and picture information linked to the keyword you've come to visit the ideal site. Our website provides you with hints for viewing the maximum quality video and picture content, search and find more enlightening video content and images that fit your interests.
comprises one of tens of thousands of video collections from various sources, particularly Youtube, therefore we recommend this movie for you to see. You can also bring about supporting this site by sharing videos and images that you enjoy on this site on your social networking accounts such as Facebook and Instagram or tell your closest friends share your experiences about the simplicity of access to downloads and the information that you get on this website. This site is for them to stop by this website.

The new system gives veterans more options for appeals after claims are denied.
Va secondary claim denied. The logic here is that the veteran is experiencing a new health problem since leaving the military that was not present at all during the time he or she served. After you have filed your claim for VA disability benefits and the VA adjudicators have decoded that your disability is service connected the Initial VA rating Once the VA has acknowledged that your disability is related to serviceie. The VA typically denies these claims reasoning that none of the conditions had their onset during service and obesity is not a disability for VA purposes. Way to do this is to provide medical records from your time on active duty showing thorough evidence of the condition especially its original diagnosis.
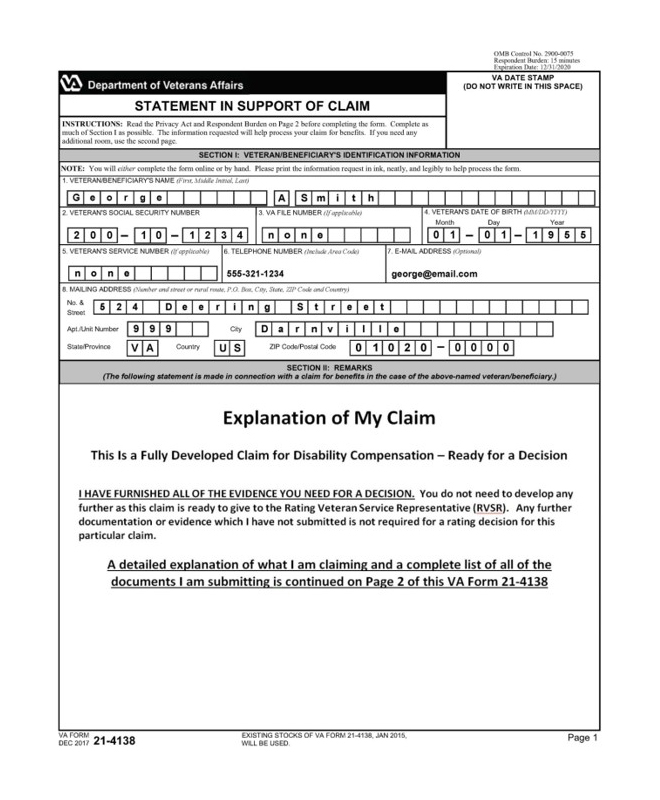
Not To Be Confused With. If youve already filed your VA disability claim and your VA claim got denied or youre underrated you likely need more medical evidence. Specifically veterans will fill out and submit VA Form 21-526 an original claim for service connection. Claiming Secondary Conditions for VA Disability For a condition to be eligible for VA Disability you must be able to prove that it is service-connected.
Read the letter the VA sent you and look specifically at the reasons why your claim was denied. Although that is generally true this particular claim can demonstrate that the physical injury during service caused weight gain a risk factor for type 2 diabetes sleep apnea and cardiovascular disease. As with any denial do not lose hope. HOW TO SUBMIT A CLAIM.
You have shown that there is was an incident in service and that you have a current disability. From a medical perspective analyze the current Department of Veterans Affairs VA practice of assigning service connection on secondary and aggravation bases. In a recent decision the US Court of Appeals for Veterans Claims affirmed the denial of a disability claim which was based on a secondary service-connected ailment. Submit your claim on a VA Form 21-526EZ.
Special claimfile a claim for special needs linked to your service-connected disability. In secondary claims determine what medical principles and practices should be applied in determining whether a causal relationship exists between two conditions. Filing a Claim for Secondary Service Connection. A VA DBQ and a Medical Nexus Letter will help you win your VA claim get service connected and obtain the VA rating and compensation you deserve in less time.
The VA calls these secondary service-connected claims These can be difficult ratings to win but not impossible. Filing a claim for secondary service connection involves the same process as filing any claim for service connection. If the Department of Veterans Affairs decides that the secondary condition warrants additional consideration for compensation it will notify the veteran and the process of adjusting your VA compensation will begin. Supplemental Claimprovide new evidence to support a disability claim that was denied.
Then send a one-sentence letter to the VA stating that you. A secondary disability claim is a condition that was caused or made worse by an already existing service-connected condition. Or you may have your claim denied if there isnt sufficient evidence or justification to approve the claim. The VA has been trying to clear its backlog of benefit claims for years.